Backgrounder

The Case for Nurse Practitioner Reform: Full Practice Authority in Pennsylvania
Key Points
- More than 580,000 Pennsylvanians live in areas with a shortage of primary care professionals relative to the population. This shortage exists throughout the state but concentrates in rural areas.
- Expanding access to primary care leads to better health outcomes, lower health care costs for consumers and taxpayers, and overall improved quality of life.
- Nurse practitioners (NPs) are highly trained health care professionals that can provide high-quality primary care at a fraction of the cost. However, regulations banning full practice authority, including full prescription authority, prevent NPs from serving patients in shortage areas.
- Allowing NPs to practice primary care independently would provide more Pennsylvanians with access to high-quality, cost-effective health care. In Maryland, full practice authority reform has led to a higher concentration of NPs, more access to care, and better health outcomes.
Primary Care Shortage
According to the Health Resources and Service Administration (HRSA), there are an estimated 98 million people living in areas without adequate access to primary care in the United States.[1] In Pennsylvania, 580,050 people live in HRSA-designated Health Professional Shortage Areas (HPSAs).[2] The primary care shortage disproportionately affects those residing in rural areas and persons of color in low-income areas.[3] To rectify this shortage, the state needs 109 additional primary care physicians in these low-access areas. Why does access to primary care matter?
- Improved health outcomes: A systematic analysis of 51 papers reveals that areas with better access to primary care see fewer avoidable hospitalizations.[4]
- Lower healthcare costs: The same systematic analysis finds that proactive care is more cost-effective than reactive care. This is because proactive care reduces hospital visits and other expensive consequences of medical issues.
- Quality of life improvements: As the Allegheny County Department of Health notes, access to health care is critical for managing chronic diseases, preventing diseases, and maintaining health.[5] When individuals are in good physical and mental health, their quality of life will also be good.
What is a Nurse Practitioner?
An NP is a health care professional who has completed intensive coursework and internship hours with clinical rotations. Their training takes six to seven years instead of the eleven to twelve years required of physicians. Aspiring NPs must qualify as registered nurses (RNs) before they can complete a graduate-level nursing program. Doctorate-level NPs typically complete an additional year of post-graduate training and complete more clinical hours. After training, all must pass a national board certification exam in their area of specialty to qualify for a license in their state.
- Though NPs do not have the same training as physicians, the health care services they provide lead to similar health outcomes for their patients.[6]
- In fact, Kaiser Permanente detailed in a 2015 issue brief findings that show NPs can perform 80–90 percent of the tasks provided by primary care physicians.[7]
What are Nurse Practitioners Allowed to do?
Each state sets laws governing the Scope of Practice (SOP) for NPs. Pennsylvania’s licensure law is the final authority for SOP in the state.[8]
SOP refers to a medical professional’s legal ability to perform specific procedures, such as referring patients to specialists, prescribing medicine, and ordering diagnostic tests. These regulations can artificially limit the care a licensed NP can provide. In other words, these NPs are underutilized. In Pennsylvania, an NP cannot practice without physician supervision, and the state limits the range of medicines they can prescribe. This is called restricted practice, short of full practice authority.
- For example, Pennsylvania NPs cannot prescribe schedule IV and III drugs for more than 90 days and schedule II drugs for more than 30 days. The NP’s collaborative agreement may further limit their prescription authority. Yet, expansive prescriptive authority is essential to providing cost-effective, quality health care.
- Pennsylvania requires an NP to either work directly for a physician or have a collaborative practice agreement. Such agreements often include a series of protocols, a schedule for the physician’s analysis of the NP’s patient charts, and the specific rights and responsibilities of the two parties. Pennsylvania’s supervision rule is especially burdensome since it requires two physicians on each collaborative practice agreement.
- These agreements are costly; an informal survey of members of the Pennsylvania Coalition of Nurse Practitioners (PCNP) finds these mandated contracts cost NPs an average of $500 to $1,000 a month.[9]
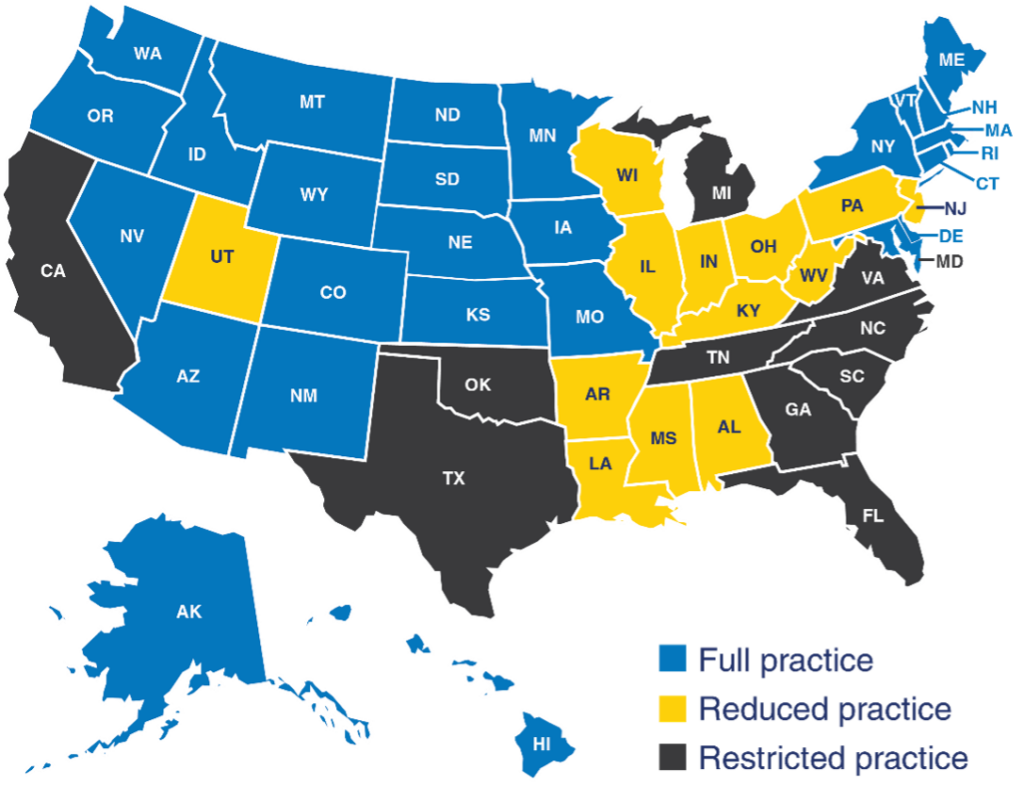
Research shows states with full practice authority for NPs have better access to primary care.[10] This is because primary care NPs are significantly more likely than primary care physicians to practice in underserved urban and rural areas.[11] Accordingly, full practice authority for NPs increases the supply of NPs in areas with few practicing physicians by 60 percent.[12] Additionally, NPs are less likely to leave states with expansive practice laws.[13] Currently, 26 states and the District of Columbia grant NPs full practice authority. An additional 13 permit reduced access, and 11 are restricted. In the past two years, four states (including New York and Delaware) moved to full practice authority for NPs.[14]
The Benefits of Full Practice Authority
The United States’ growing primary care shortage affects the quality and cost of care, which, in turn, impacts quality of life. Giving NPs full practice authority would help rectify this shortage and would represent a win-win-win solution to health care access problems. Consider the benefits of reform for patients, physicians, and governments:
Patients
- Better Health: Increased access to primary care—especially by the poor, people of color, and those in rural communities—will result in better management of chronic diseases, fewer hospitalizations, and higher quality of life. In Maryland the reform has met great success:
- After granting full practice authority in 2015, Maryland’s NP density more than doubled. Maryland border counties have 22.4 more NPs per 100,000 people than Pennsylvania border counties.
- If Pennsylvania adopted the same reform our research estimates Pennsylvanians could see a 29.5 percent increase in the number of NPs. Furthermore, Pennsylvanians can expect to see better health outcomes because of increased access to care. Our research finds granting full practice authority would allow the commonwealth a 7 percent reduction in poor mental health days and a 15 percent decrease in people reporting poor or fair health.[15]
- Lower Costs: Better disease management and fewer hospitalizations drive health care costs down.
- Personalized Care: An ample supply of primary care providers will allow patients to spend more time with their health care provider. Moreover, patients will have greater choice in health care settings. For example, in Maryland, NPs open offices specializing in senior care and provide home visits.
- Polling shows that patients support full practice authority. A Morning Consult survey of recent health care patients finds that 82 percent support full practice authority for NPs.[16]
Physicians
- Physicians will be able to focus on providing high-value, complex care.
- survey shows NPs as the most sought-after medical staff. Meanwhile, full practice authority has proven to attract more NPs to a state. Thus, it is reasonable to conclude that full practice authority could help staff doctors’ offices.[17]
Governments
- The increased supply of providers will decrease the expenses (in part paid by the government) associated with patients who go to the emergency room because they cannot get a primary care appointment.[18]
- In 2019, the Journal of Nursing Regulation published findings that full practice authority reduces Medicaid spending for several measures.[19]
Myths and Facts: Quality
- Myth: With their additional training, physicians provide more accurate diagnoses and effective treatments.
- Fact: A systematic analysis of 34 years of research finds that NPs provide “cost-effective care with patient outcomes that are equivalent to or better than usual care and with lower costs.”[20] Another study reveals that the care patients receive from NPs and physicians is not significantly different in quality, even after accounting for differences among state SOP regulations.[21]
- Myth: NPs may be able to handle the easiest cases, but complex cases require physicians with additional training.
- Fact: An analysis of Medicare patient data found that NPs and physician assistants (PAs) provide similar care for all but the rarest conditions.[22] Overall, research finds no evidence that licensing restrictions affect care quality and patient safety.[23]
Myths and Facts: Cost-Effectiveness
- Myth: Full practice authority would be fiscally irresponsible due to increased Medicaid costs.
- Fact: Full practice authority reduces costs to state governments because (1) Payments to NPs tend to be 85 percent of payments to physicians and (2) increased primary care in general saves money in the long run.[24] A Health Policy published study finds that “allowing PAs to prescribe controlled substances is associated with a substantial (more than 11 percent) reduction in the dollar amount of outpatient claims per Medicaid recipient.”[25]
- Myth: Greater access to primary care increases costs due to more utilization.
- Fact: An expansive review of the literature finds that better access to care reduces patient complications including hospitalizations, which saves costs.[26]
- Myth: Full practice authority has no effect on health care costs.
- Fact: Multiple studies show that NPs and PAs provide quality primary care at a lower cost. Patients assigned to physicians or NPs in the Veterans Administration have similar clinical outcomes, similar diagnostic tests, and similar costs.[27] Another study of Veterans Affairs patients with complex medical issues finds that case-mix-adjusted total care costs are 6–7 percent lower for NP and PA patients than for physician patients.[28] Furthermore, NPs could reduce the costs of well-child checkups by 10 percent, saving consumers $600 million annually.[29]
Myth and Facts: Access to Care
- Myth: NPs are more likely to practice in the same geographic locations as physicians, so full practice authority will not mitigate provider shortages in rural areas.
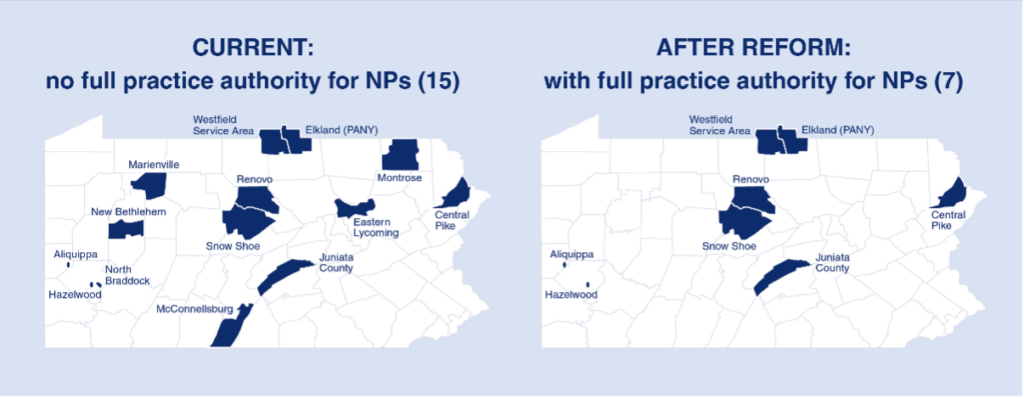
- Fact: Research demonstrates that NPs are more likely than physicians to work in rural areas, where access to care shortages is most critical.[30] If Pennsylvania had the same density of NPs as Maryland and all of them focused on primary care, we could eliminate half of our largely rural geographic health care provider shortage areas.[31]
- Myth: Increasing providers will not address underlying issues that led to the current shortage.
- Fact: State regulations have a large impact on retail health clinics’ ability to implement innovations. Increased use of NPs is likely to spur innovation in health care delivery.[32] For example, clinics staffed with NPs and other advanced practice registered nurses (APRNs) generally offer weekend and evening hours.
Conclusion
Pennsylvania is facing a critical shortage of health care access in rural and low-income areas. Access to primary care is vital for physical health and overall quality of life. Regular primary care visits also decrease the likelihood of avoidable hospital trips and avoidable deaths. Fortunately, NPs can provide high-quality health care services to populations with low access to health care. NPs are cost-effective and more likely than physicians to serve populations with low access to care.
However, the government limits how much NPs can serve Pennsylvanians. Currently, NPs do not have full prescriptive authority and are unable to work without physician supervision. Full practice authority for NPs gives them the ability to practice independently and without undue restrictions. With one licensing reform lawmakers can provide low-income and rural Pennsylvanians with better access to high-quality, cost-effective health care.
[1]Health Resources and Services Administration (HRSA), “Health Workforce Shortage Areas,” accessed October 11, 2022, https://data.hrsa.gov/topics/health-workforce/shortage-areas.
[2]Health Resources and Services Administration (HRSA), “Designated Health Professional Shortage Areas Statistics,” September 30, 2022, https://data.hrsa.gov/Default/GenerateHPSAQuarterlyReport.
[3]Amelia Goodfellow, et al., “Predictors of Primary Care Physician Practice Location in Underserved Urban or Rural Areas in the United States: A Systematic Literature Review,” Academic Medicine: Journal of the Association of American Medical Colleges 91, No. 9 (September 2016) 1313–21, https://doi.org/10.1097/acm.0000000000001203.
[4]Aldo Rosano, et al., “The Relationship between Avoidable Hospitalization and Accessibility to Primary Care: A Systematic Review,” European Journal of Public Health 23, No. 3 (June 2013) 356–60, https://doi.org/10.1093/eurpub/cks053.
[5]Allegheny County Health Department, “Health Equity Brief Access to Health Care in Allegheny County,” May 2018, https://www.alleghenycounty.us/uploadedFiles/Allegheny_Home/Health_Department/Resources/Data_and_Reporting/Chronic_Disease_Epidemiology/HEB-ACCESS.pdf.
[6]Jeffrey Traczynski and Victoria Udalova, “Nurse Practitioner Independence, Health Care Utilization, and Health Outcomes,” Journal of Health Economics 58, (March 2018) 90–109, https://doi.org/10.1016/j.jhealeco.2018.01.001.
[7]Amanda Van Vleet and Julia Paradise, “Tapping Nurse Practitioners to Meet Rising Demand for Primary Care,” Kaiser Family Foundation, January 20, 2015, https://www.kff.org/medicaid/issue-brief/tapping-nurse-practitioners-to-meet-rising-demand-for-primary-care/.
[8]49 Pa. Code § 21, “Chapter 21. State Board of Nursing,” accessed October 11, 2022, https://www.pacodeandbulletin.gov/Display/pacode?file=/secure/pacode/data/049/chapter21/chap21toc.html&d=reduce.
[9]Christen Smith, “Collaborative Agreements with NPs Can Generate Thousands for PA Physicians,” CapitolWire, May 21, 2015, https://www.pacnp.org/news/news.asp?id=232876.
[10]Kevin Stange, “How Does Provider Supply and Regulation Influence Health Care Markets? Evidence from Nurse Practitioners and Physician Assistants,” Journal of Health Economics 33 (January 2014) 1–27, https://doi.org/10.1016/j.jhealeco.2013.10.009.
[11]Peter Buerhaus, et al., “Practice Characteristics of Primary Care Nurse Practitioners and Physicians,” Nursing Outlook 63, No. 2 (March–April 2015) 144–53, https://doi.org/10.1016/j.outlook.2014.08.008.
[12]Benjamin McMichael, “Beyond Physicians: The Effect of Licensing and Liability Laws on the Supply of Nurse Practitioners and Physician Assistants,” Journal of Empirical Legal Studies 15 (October 2018) 732–71, https://doi.org/10.1111/jels.12198.
[13]Shishir Shakya and Alicia Plemmons, “Does Scope of Practice Affect Mobility of Nurse Practitioners Serving Medicare Beneficiaries?” July 14, 2020, http://dx.doi.org/10.2139/ssrn.3651399
[14]American Association of Nurse Practitioners, “State Practice Environment Map,” accessed October 11, 2022, https://www.aanp.org/advocacy/state/state-practice-environment.
[15]Kihwan Bae, et al., “Maryland’s Healthcare Lesson for Pennsylvania: How Full Practice Authority Can Increase Access to Care and Improve Health Outcomes,” Commonwealth Foundation, November 15, 2022, https://www.commonwealthfoundation.org/research/full-practice-authority-pennsylvania/.
[16]Morning Consult, “Telehealth for Health Care Practitioners & Consumers,” April 2022, https://connectwithcare.org/wp-content/uploads/2022/04/Telehealth_MC-Branded_PPT_Final.pdf.
[17]Bae, et al., “Maryland’s Healthcare Lesson for Pennsylvania.”
[18]Jeffrey Traczynski and Victoria Udalova, “Nurse Practitioner Independence, Health Care Utilization, and Health Outcomes,” Journal of Health Economics 58 (March 2018) 90–109, https://doi.org/10.1016/j.jhealeco.2018.01.001.
[19]L. Poghosyan, et al., “The Economic Impact of the Expansion of Nurse Practitioner Scope of Practice for Medicaid,” Journal of Nursing Regulation 10, No. 1 (April 2019) 15–20, https://doi.org/10.1016/S2155-8256(19)30078-X.
[20]Ruth Martin-Misener, et al, “Cost-effectiveness of Nurse Practitioners in Primary and Specialised Ambulatory Care: Systematic Review,” BMJ Open 5, No. 6 (May 2015), doi: 10.1136/bmjopen-2014-007167, https://bmjopen.bmj.com/content/bmjopen/5/6/e007167.full.pdf.
[21]Ellen T. Kurtzman, et al., “Does the Regulatory Environment Affect Nurse Practitioners’ Patterns of Practice or Quality of Care in Health Centers?” Health Services Research 52 Suppl 1 (February 2017) 437–58, https://doi.org/10.1111/1475-6773.12643.
[22]Danny R. Hughes, et al., “A Comparison of Diagnostic Imaging Ordering Patterns between Advanced Practice Clinicians and Primary Care Physicians Following Office-Based Evaluation and Management Visits,” JAMA Internal Medicine 175, No.1 (2015) 101–7, https://doi.org/10.1001/jamainternmed.2014.6349.
[23]Morris M. Kleiner, et al., “Relaxing Occupational Licensing Requirements: Analyzing Wages and Prices for a Medical Service,” Journal of Law and Economics 59, No. 2 (May 2016) 261–91, https://doi.org/10.1086/688093.
[24]Laura Barrie Smith, “The Effect of Nurse Practitioner Scope of Practice Laws on Primary Care Delivery,” Health Economics 31, No. 1 (January 2022) 21–41, https://doi.org/10.1002/hec.4438.
[25]Edward Joseph Timmons, “The Effects of Expanded Nurse Practitioner and Physician Assistant Scope of Practice on the Cost of Medicaid Patient Care,” Health Policy 121, No. 2 (February 2017) 189–96, https://doi.org/10.1016/j.healthpol.2016.12.002.
[26]Rosano et al, “The Relationship Between Avoidable Hospitalization.”
[27]Chuan-Fen Liu, et al., “Outcomes of Primary Care Delivery by Nurse Practitioners: Utilization, Cost, and Quality of Care,” Health Services Research 55, No. 2 (April 2020) 178–89, https://doi.org/10.1111/1475-6773.13246.
[28]Perri A Morgan, et al., “Impact of Physicians, Nurse Practitioners, and Physician Assistants on Utilization and Costs for Complex Patients,” Health Affairs 38, No. 6 (June 2019) 1028–36, https://doi.org/10.1377/hlthaff.2019.00014.
[29]Kleiner, et al., “Relaxing Occupational Licensing Requirements.”
[30]Kevin Grumbach, et al, “Who Is Caring for the Underserved? A Comparison of Primary Care Physicians and Nonphysician Clinicians in California and Washington,” Annals of Family Medicine 1, No. 2 (July 2003) 97-104, https://doi.org/10.1370%2Fafm.49.
[31]Bae, et al., “Maryland’s Healthcare Lesson for Pennsylvania.”
[32]Aaron Hoffman, “Minute Medicine: Examining Retail Clinic Legal Issues and Legislative Challenges,” Journal of Law-Medicine 20, No. 2 (2020) 467–97, https://scholarlycommons.law.case.edu/cgi/viewcontent.cgi?article=1152&context=healthmatrix.