Report

How Full Practice Authority Can Increase Access and Improve Outcomes
Key Findings
- Marylanders in border counties have better health care outcomes, including fewer residents reporting fair or poor health and fewer residents with poor mental health days.
- Before full practice authority, Maryland had more Nurse Practitioner (NP) density than Pennsylvania, but the gap doubled after Maryland’s reform while physician density remained constant.
- Based on Maryland’s experience, full practice authority would increase the number of Certified Nurse Midwives (CNMs) in Pennsylvania by an estimated 26.7 percent, and the number of NPs by 29.5 percent.
- Allowing full practice authority would increase the number of patients seen by NPs per week by 1,792 patients.
- Full practice authority could, if all NPs focus on primary care, eliminate nearly half of Pennsylvania’s geographic Health Professional Shortage Areas (HPSAs).
Executive Summary
Despite numerous healthcare reforms, the United States faces a shortage of primary care physicians, and Pennsylvania is no exception. The national physician shortage is projected to grow between 21,400 and 55,200, limiting healthcare access for patients.[1]
Areas with a shortage of primary care professionals relative to the population are classified as Health Professional Shortage Areas (HPSAs). As of June 2022, Pennsylvania included 148 areas designated as HPSAs, covering some or all 20 counties and 580,050 residents.[2]
Difficulty accessing primary care is not just an inconvenience; regular access to healthcare providers is well-documented to positively impact health and quality of life.[3] Long travel distances and long wait times cause people to delay or forego care entirely, allowing conditions to worsen.
Healthcare access presents a unique challenge for Pennsylvania. HPSAs exist in rural and urban areas, and the reforms designed to resolve HPSAs in one area may not be effective for others.
Skilled professionals, like Advanced Practice Registered Nurses (APRNs), can help fill the gap. However, current state laws often prevent skilled APRNs from providing primary care to patients. State Scope of Practice (SOP) laws govern APRNs, limiting what tasks they can perform. These laws define each provider’s role and dictate the oversight they must have to practice.
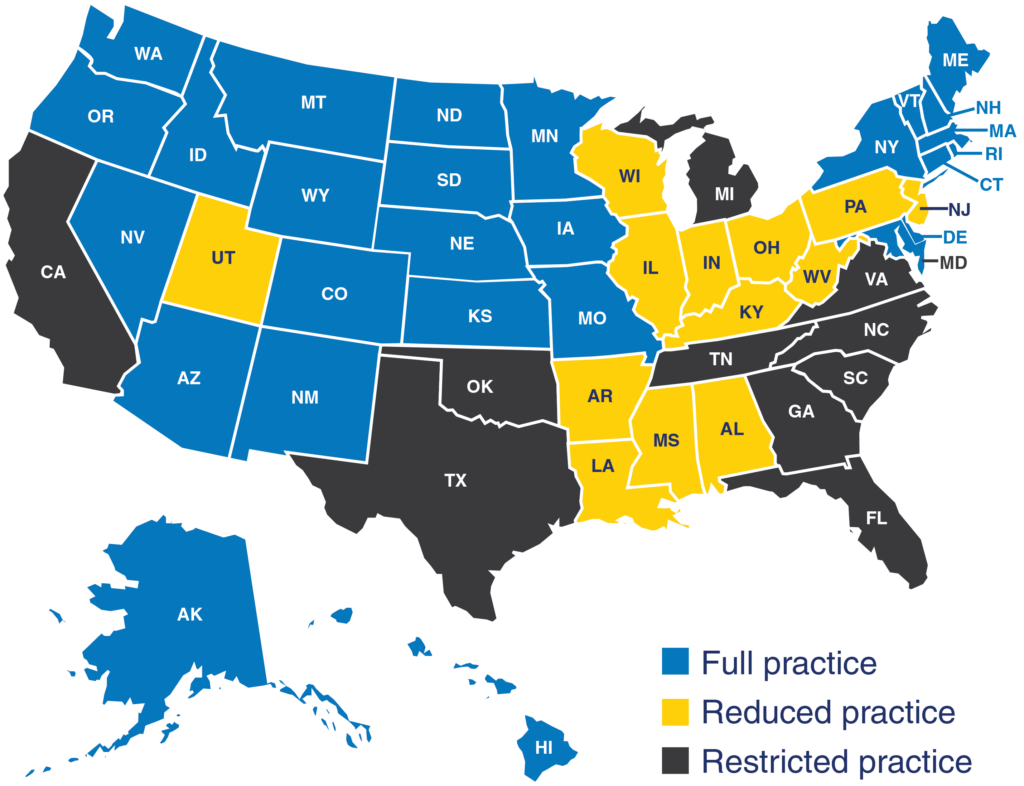
For example, in Pennsylvania, APRNs must collaborate with physicians, limiting where and how they practice. In contrast, the District of Columbia and twenty-six states, including Maryland, Delaware, and New York, allow APRNs full practice authority, or the ability to practice independently.
APRNs are registered nurses (RNs) with an advanced degree—Masters or post-Masters level.[4] They have the training to provide many primary care services traditionally performed by physicians. Full practice authority would allow APRNs to practice to the full extent of their education and training, using their skills and ability to increase access for patients in medically underserved areas.
In this report, we first review empirical evidence on the potential benefits of APRNs with full practice authority. We then compare the southern Pennsylvania border to the northern Maryland border to show the effect of moving to full practice authority for two types of APRNs: Nurse Practitioners (NPs) and Certified Nurse Midwives (CNMs).
We estimate that allowing full practice authority in Pennsylvania would increase the number of CNMs by 0.6 per 100,000 residents (26.7 percent) and increase the number of NPs by 22.4 per 100,000 residents (29.5 percent).
We also explore the effect that an increase in the number of NPs and CNMs would have on patient outcomes. We estimate that full practice authority in Pennsylvania would decrease the share of residents who report being in poor or fair health by 2.8 percentage points (14.9 percent) and reduce poor mental health days by 0.354 days per person (7.2 percent). Our analysis suggests that Pennsylvania moving to full practice authority will improve access to care for residents and thus help improve health outcomes.
Download the full report here.
[1]IHS Markit Ltd, “The Complexities of Physician Supply and Demand: Projections From 2018 to 2033,” (Washington D.C.: American Association of Medical Colleges, June 2020), https://www.aamc.org/system/files/2020-06/stratcomm-aamc-physician-workforce-projections-june-2020.pdf.
[2]Health Workforce Health Resources and Services Administration (HRSA), “Fourth Quarter of Fiscal Year 2022 Designated HPSA Quarterly Summary,” U.S. Department of Health and Human Services (HHS), September 30, 2022, https://data.hrsa.gov/Default/GenerateHPSAQuarterlyReport.
[3]Ani Bilazarian, et al., “Primary Care Practice Structural Capabilities in Health Professional Shortage Areas,” American Journal of Managed Care 28, No. 5 (2022) 212–17, https://doi.org/10.37765/ajmc.2022.89142.
[4]National Council of State Boards of Nursing (NCSBN), “APRNs in the U.S.,” accessed October 12, 2022, https://www.ncsbn.org/aprn.